Fatigue in Aviation—More Than Just Jet Lag

Dr. Jaime Devine
Associate Scientist, Operational Fatigue and Performance, Institute for Behavior Resources, Inc. Baltimore, Maryland, United States of America
Fatigue Factors in Medium Haul Aviation
Pilot fatigue constitutes a well-acknowledged threat to aviation safety. The bulk of research on fatigue in aviation has concentrated on long haul operations during which pilots must cross multiple time zones. Because jet lag and nighttime operations are major fatigue factors for long haul [1], fatigue in aviation is routinely viewed as an issue resulting solely from sleep deprivation or circadian disruption.
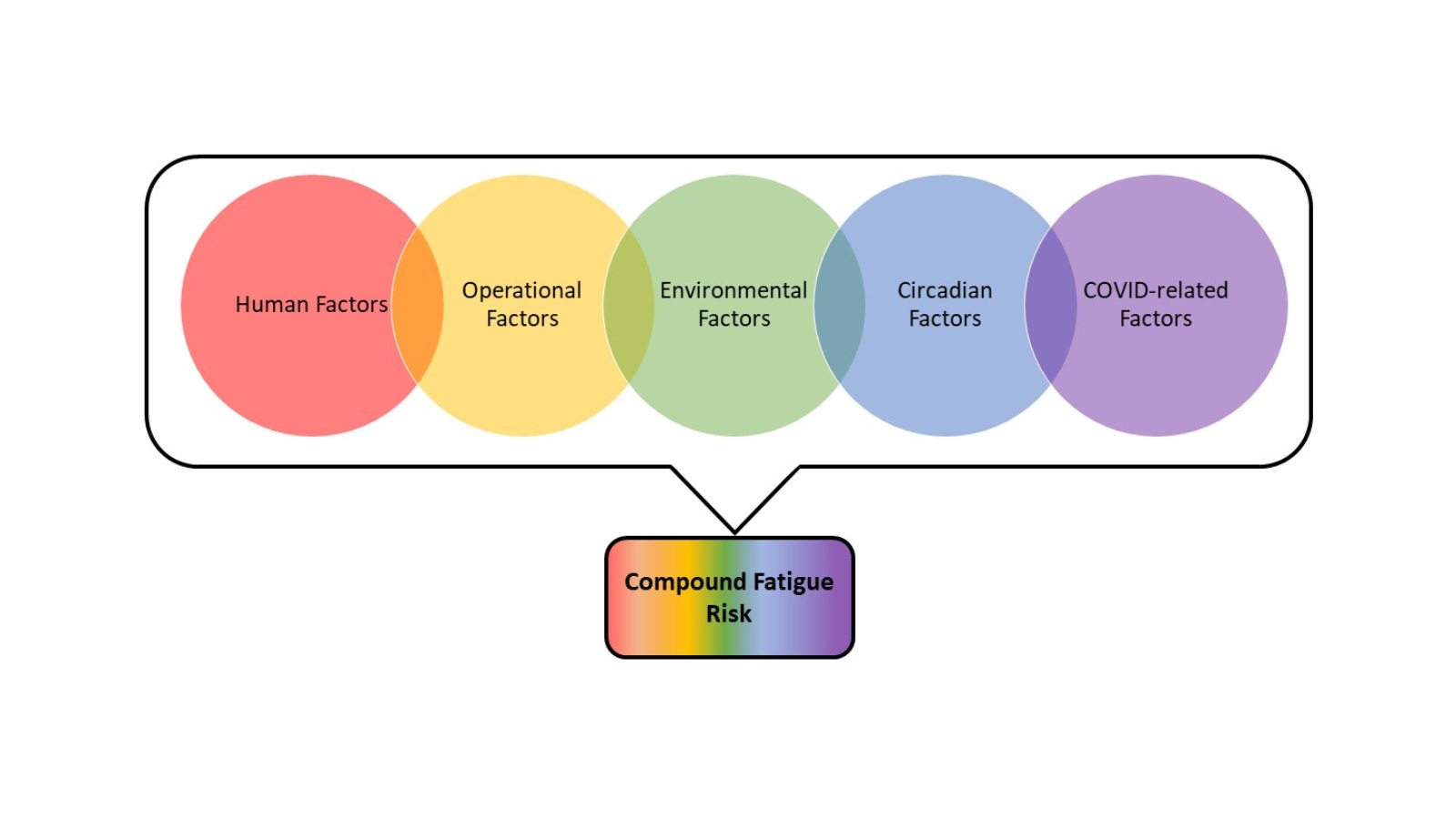
Conversely, medium haul operations are typified by multiple flight segments per day lasting less than 8 hours each and crossing less than three time zones [2, 3]. Fatigue factors in medium haul aviation are more commonly thought of as being related to workload factors rather than to jet lag or sleep disruption [1-4]. Sleep disruption is a serious source of fatigue for pilots, but pilots may also experience mental or emotional fatigue due to interpersonal relationships with their co-workers or in response to COVID-related precautions like mask-wearing. Environmental factors like noise or weather can increase the risk of fatigue as well. Fatigue mitigation strategies can be improved by understanding how factors combine to create an elevated period of risk for the pilot.
In an anonymous online survey, pilots working medium-haul rosters for a major European airline were asked to rank the level of fatigue they experience from 38 separate factors across five domains: 1) Human; 2) Operational; 3) Environmental; 4) Circadian/Biological; and 5) COVID-related. These rankings provide targets for scheduling interventions to avoid periods of compound fatigue risk.
Compound Fatigue Risk and Biomathematical Modeling
Fatigue factors from different domains are not mutually exclusive. As an example, a pilot may cut sleep short to report for an early schedule, experience flight delays and foul weather while wearing a mask to prevent the spread of COVID-19 and working with an uncooperative co-pilot. It is possible that incremental amounts of fatigue from each individual factor in this scenario could combine to create a greater overall compound fatigue risk.
Prospective fatigue evaluation tools like biomathematical models of fatigue (BMMF) predict fatigue as a function of the three-process model (TPM), with the three processes being sleep need, time of day, and sleep inertia [5-7]. At least one BMMF, the Sleep, Activity, Fatigue, and Task Effectiveness Fatigue Avoidance Scheduling Tool (SAFTE-FAST) [7], can also model fatigue due to workload. Workload is considered separate from biological impairment due to circadian misalignment or sleep debt in SAFTE-FAST. Fatigue factors from the medium haul pilot survey that could be predicted using a BMMF are being incorporated into SAFTE-FAST as weighted workload factors with the goal of identifying proposed pilot schedules with high compound fatigue risk.
Better Safe Than Sorry
Schedules where workload is high at the same time that an operator can be expected to be impaired due to sleep or circadian factors should be considered particularly hazardous to safety. That is not to say that a safety incident will necessarily occur during such a time, but rather, that there is an increased likelihood of an event occurring. Avoiding periods of potential high risk are crucial in the operational environment. Applied science approaches like modeling compound fatigue risk are essential to the prevention of adverse events in real-world environments.
Check out Jaime Devine’s ePoster on “The role of rank and sleep debt on compound fatigue risk in medium haul pilots presented” at Sleep Europe 2022, by logging in to the virtual platform.
References
- Powell, D.M., et al., Pilot fatigue in short-haul operations: effects of number of sectors, duty length, and time of day. Aviat Space Environ Med, 2007. 78(7): p. 698-701.
- Roach, G.D., et al., Duty periods with early start times restrict the amount of sleep obtained by short-haul airline pilots. Accid Anal Prev, 2012. 45 Suppl: p. 22-6.
- Gander, P.H., et al., Flight crew fatigue II: short-haul fixed-wing air transport operations. Aviat Space Environ Med, 1998. 69(9 Suppl): p. B8-15.
- Alcéu, P.M.d.M., Managing fatigue in a regional aircraft operator: fatigue and workload on multi-segment operations. 2015.
- Mallis, M.M., et al., Summary of the key features of seven biomathematical models of human fatigue and performance. Aviat Space Environ Med, 2004. 75(3 Suppl): p. A4-14.
- Åkerstedt, T. and S. Folkard, Validation of the S and C Components of the Three-Process Model of Alertness Regulation. Sleep, 1995. 18(1): p. 1-6.
- Hursh, S.R., et al., Fatigue models for applied research in warfighting. Aviation, space, and environmental medicine, 2004. 75(3): p. A44-A53.
ESRS Reminders
2023 Sleep Medicine Examination
Recent publications from ESRS members
- Bosch et al. (2022). Dexmedetomidine in Psychiatry: Repurposing of its Fast-Acting Anxiolytic, Analgesic and Sleep Modulating Properties. Pharmacopsychiatry.
- Thorarinsdottir et al. (2022). Evaluation of excessive daytime sleepiness in obstructive sleep apnea across international sleep centers. Sleep.
- Juan et al. (2022). Distinct signatures of loss of consciousness in focal impaired awareness versus tonic-clonic seizures. Brain.
- Weihs et al. (2022). The relationship between Alzheimer’s-related brain atrophy patterns and sleep macro-architecture. Alzheimers Dement (Amst).
- Tranfić Duplančić et al. (2022). Salivary parameters and periodontal inflammation in obstructive sleep apnoea patients. Sci Rep.
- Stokes et al. (2022). Quality-adjusted life years for digital cognitive behavioural therapy for insomnia (Sleepio): a secondary analysis. BJGP Open.
- Garbazza et al. (2022). Influence of chronotype on the incidence and severity of perinatal depression in the “Life-ON” study. J Affect Disord.
- Pérez-Carbonell et al. (2022). Sleep architecture and sleep-disordered breathing in fatal insomnia. Sleep Medicine.
- Habib et al. (2022). Performance of a Convolutional Neural Network Derived from PPG Signal in Classifying Sleep Stages. IEEE Trans Biomed Eng.
- Blackman et al. (2022). Cross-sectional and longitudinal association of sleep and Alzheimer biomarkers in cognitively unimpaired adults. Brain Commun.