Sleep Science Monday: Sleep in the time of COVID
Sleep Science Monday: Sleep in the time of COVID
Better late than never! It’s the start of another week—grab a coffee/tea/beer/wine and begin your week with a quick recap of Sleep Science News and ESRS updates!
5 October 2020
Moving into shorter and colder days (here in the northern hemisphere), flu season is on the horizon as countries already battle second waves of COVID-19. Experts remind us to stay conscientious and continue practicing social distancing, wearing masks, limiting travel, and maintaining proper hygiene (wash your hands!). Additionally, don’t underestimate the importance of a good night’s sleep. Highlighted in Emily Sohn’s recent National Geographic article, the relationship between sleep and COVID-19 is succinctly summarized as “Want to reduce your COVID-19 risk? You need to sleep more.”
Although the exact mechanisms are still being explored, sleep is linked with the body’s immune response and ability to fight infections—with less and poorer quality sleep related to higher rates of respiratory diseases and other illness. This may not come as a surprise, as numerous studies have already linked poor sleep with an array of health risks, from cancer (Hurley et al., 2020), neurodegenerative diseases (Lucey et al., 2020), cardiovascular diseases (Sun et al., 2020), sleep-disordered breathing (Maas et al., 2020), and mental disorders (Peng et al., 2020). Furthermore, these health conditions also increase COVID-19 susceptibility, with worse outcomes. In turn, those with COVID-19 have poorer quality sleep and more daytime fatigue—creating a feedback loop leading to a diminished ability to fight off the disease.
Lack of sleep also reduces antibody response to certain vaccines, leading to some concerns on the effectiveness of a COVID-19 vaccination in those that already experience sleep disorders, frontline healthcare workers (Cai et al., 2020; Khanal et al., 2020), and shift workers. Additionally, trying to get enough sleep before and after receiving the vaccination may by a straightforward way to increase its effectiveness.
Indeed, during the pandemic, many experienced increased psychological distress (Rheenan et al., 2020), as well as altered sleep habits (Niedzwiedz et al., 2020) and circadian rhythms (Morin et al., 2020). This is particularly concerning as a recent Audit by the British Sleep Society found that COVID-19 also had a significant and negative impact on UK sleep services as staff were redeployed, moved to home office, furloughed, or off due to illness.
Therefore, managing sleep behaviors is particularly important during these stressful times. For those experiencing more severe sleep disturbances, such as chronic insomnia, exploring the possibility of CBT-I (cognitive behavioral therapy for insomnia) with your doctor could help to alleviate some symptoms. For others, practicing good sleep hygiene (e.g., meditation, limiting screen time, developing a schedule) may prove a simple strategy to improve the body’s ability to stay healthy and fight off infections.
_____________________________
For recent publications on other sleep and sleep-related research and medicine:
- Adawi et al. (2020) Sleep disorders and vascular responsiveness in patients with rheumatoid arthritis
- Bothe et al. (2020) Gross motor adaptation benefits from sleep after training
- Clark et al. (2020) Effects of orexin receptor antagonism on human sleep architecture: A systematic review
- Groenewald et al. (2020) Associations between adolescent sleep deficiency and prescription opioid misuse in adulthood
- Jiménez-Jiménez et al. (2020) Sleep disorders in Tourette syndrome
- Lancel et al. (2020) Sleep disturbances in bereavement: A systematic review
- Liu et al. (2020) Risk factors associated with mental illness in hospital discharged patients infected with COVID-19 in Wuhan, China
- Mahalakshmi et al. (2020) Sleep, brain vascular health and ageing
- Matenchuk et al. (2020) Sleep, circadian rhythm, and gut microbiota
- Markovic et al. (2020) Gender differences in adolescent sleep neurophysiology: a high-density sleep EEG study
- Mead and Irish (2020) Application of health behaviour theory to sleep health improvement
- Mylonas et al. (2020) Naps reliably estimate nocturnal sleep spindle density in health and schizophrenia
- Pamidi et al. (2020) Optimal Continuous Positive Airway Pressure Treatment of Obstructive Sleep Apnea Reduces Daytime Resting Heart Rate in Prediabetes: A Randomized Controlled Study
- Raven et al. (2020) Sleep deprivation‐induced impairment of memory consolidation is not mediated by glucocorticoid stress hormones
- Selvanathan et al. (2020) Sleep-disordered breathing in patients on opioids for chronic pain
- Shriane et al. (2020) Sleep hygiene in shift workers: A systematic literature review
- Zhang et al. (2020) Sleep problems in Rett syndrome animal models: A systematic review
_____________________________
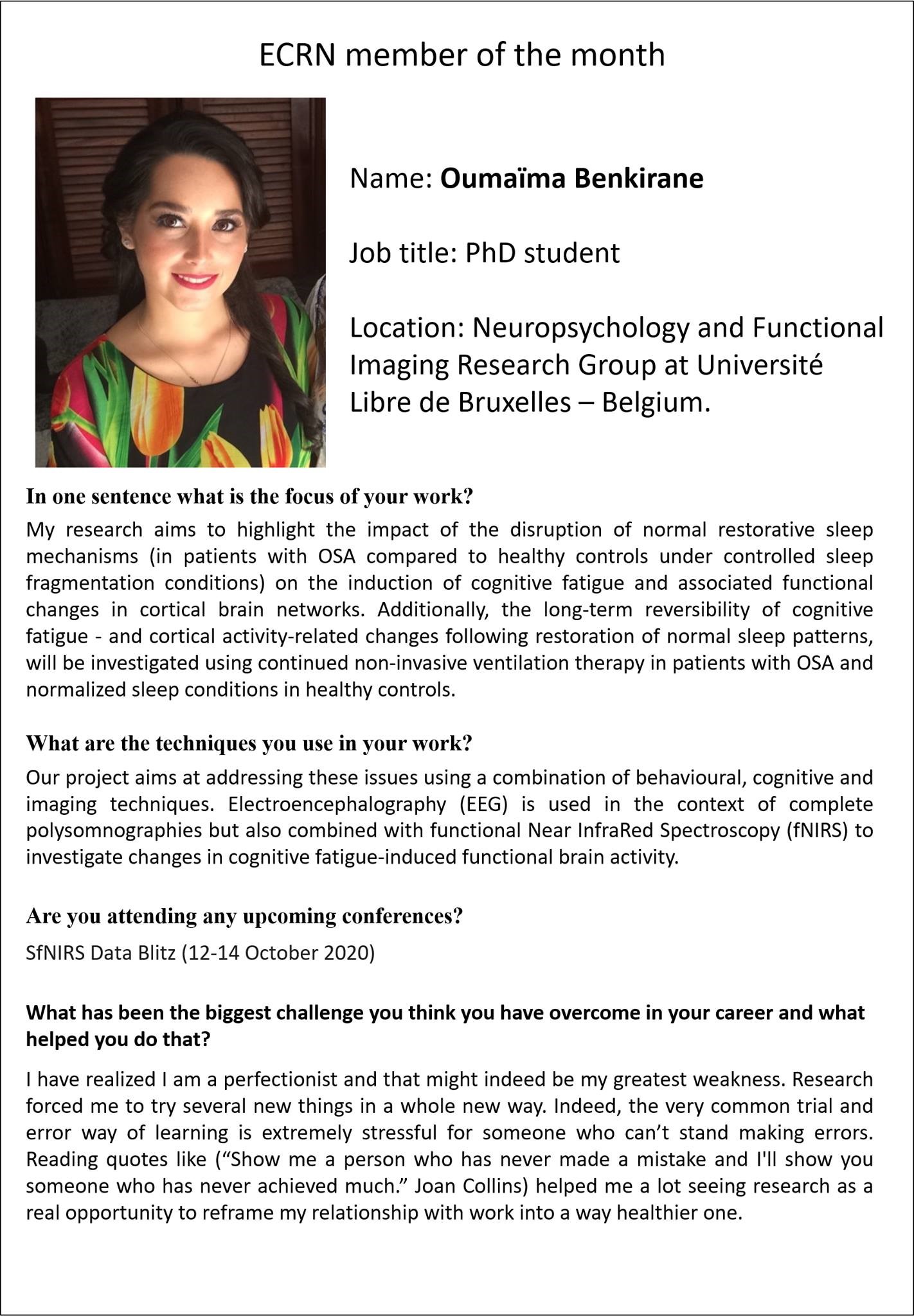
We would like to highlight ESRS Early Career Researcher, Oumaïma Benkirane, as our September ECRN member of the month.
Are you interested in or working on sleep and sleep-related research and medicine?
Attendees of the virtua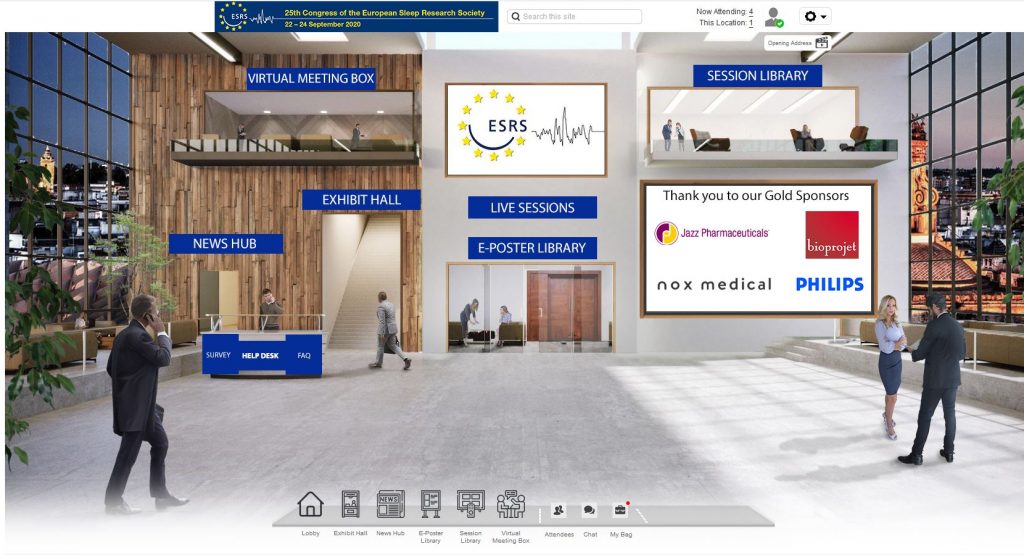 l edition of the 25th Congress of the ESRS (22 – 24 Sept 2020) still have access to all our amazing talks and posters online until the end of the month! Our organizers would also like to get your feedback as this was a novel experience for us as well. Tells us your thoughts by filling out the Survey at the Help Desk in the Lobby. For those who were unable to attend, stay tuned as we work on making the Congress more widely available.
l edition of the 25th Congress of the ESRS (22 – 24 Sept 2020) still have access to all our amazing talks and posters online until the end of the month! Our organizers would also like to get your feedback as this was a novel experience for us as well. Tells us your thoughts by filling out the Survey at the Help Desk in the Lobby. For those who were unable to attend, stay tuned as we work on making the Congress more widely available.
Due to COVID-19, the Clinical Update Sleep 2020 is postponed until next spring, 19 March 2021. However, don’t miss out on the opportunity to join their free webinar on 16 October 2020. The webinar will cover topics on sleep, COVID-19, insomnia, cardiorespiratory interactions in sleep apnea, and highlights from the sleep-focused issue of the Journal of Thoracic Disease.
We are also very excited to co-organize the Sleep and Breathing 2021 conference (15-17 April) with the European Respiratory Society. #SleepBreathe2021 will be a mixed virtual and in-person conference in Prague (although this is subject to change depending on the pandemic). The scientific program is available and abstract submissions are open until Friday 30 October 23:59 CEST. We look forward to receiving your submissions.
Have a great week!
Just published an article? Want your research to be featured? Saw something interesting? Contact: doris.wu [ at ] esrs.eu.
Not a member of ESRS? Apply here and see our wide range of benefits, including a yearly online subscription to the Journal of Sleep Research, automatic membership to the Federation of European Neuroscience Societies (FENS), support for early career researchers via the ECRN, regular updates via the ESRS Newsletter, promotion of your research, and more.