Sleep and Alzheimer’s: “Ich habe mich verloren”
Sleep Science Friday
Yes! It’s Friday! Grab a coffee/tea/beer/wine and end your week with a quick recap of Sleep Science News and ESRS updates!
“Ich habe mich verloren.”
– Auguste Deter (16 May 1850 – 8 April 1906)
Exhibiting paranoid and erratic behavior, delusions, and issues with speech and memory, 51-year-old Auguste Deter was examined by German neurologist, Dr. Alois Alzheimer, at the Frankfurt Institution of the Mentally Ill and Epileptics (Germany). Given her young age, Dr. Alzheimer initially labelled her condition as “presenile dementia”. Over the next several years, living in a state of confusion that progressively deteriorated, she soon lost sense of time and space—unable to recall her husband, where she was, and her own name—frequently uttering, “I have lost myself”. In this way, the loss of memory is a loss of self.
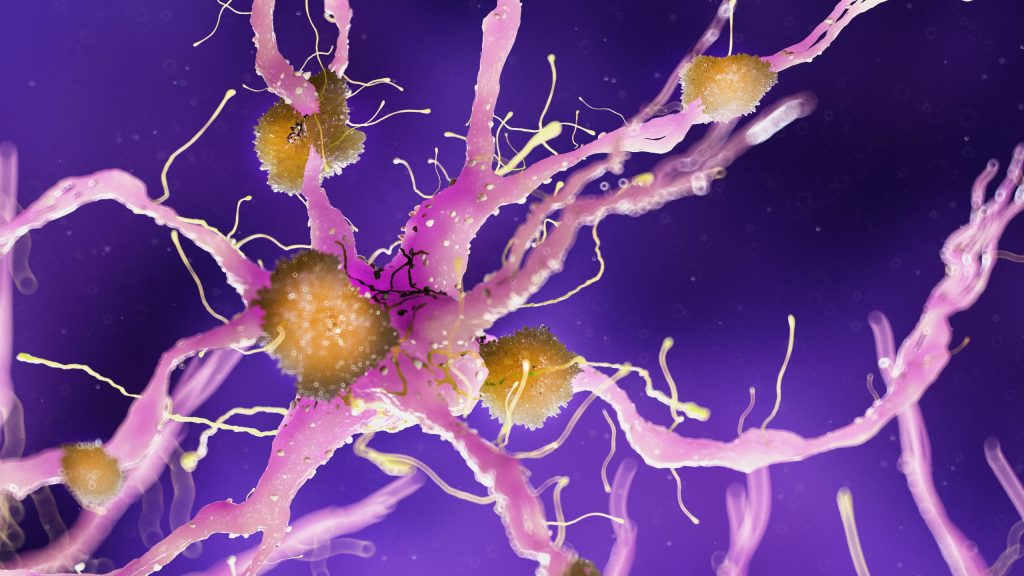
Upon her premature death five years later, Dr. Alzheimer examined thin slices of Ms. Deter’s brain—discovering two peculiar changes now recognized as amyloid plaques and neurofibrillary tangles. Ms. Deter became the first known patient with (what was later named) Alzheimer’s disease, or the “disease of forgetting”.
Since then, additional neurophysiological characteristics of Alzheimer’s and other neurodegenerative diseases have been discovered. As no cure exists, recognizing signs of mild cognitive impairment with atypical physiological ageing of the brain is necessary for early diagnosis and treatment to slow its course. One promising avenue for this is found within sleep research.
Dr Kristine Yaffe, a professor of psychiatry, neurology and epidemiology at the University of California, San Francisco, remarked, “There has been a real renaissance in research around the connection between sleep, sleep quality, sleep disturbance and dementia, especially Alzheimer’s dementia”.
Besides having a physically restorative role and effect on mental health, memory, and learning, researchers also found that the brain remains surprisingly active during sleep—and not just to dream. In 2009, a strong link was found between lack and quality of sleep with the build-up of amyloid plaques. This relationship turns out to be bidirectional, where those with amyloid plaques and still normal cognitive function also reported sleep issues. Following this, the discovery of the “glymphatic system” showed that remarkably, the brain essentially cleanses itself during sleep by washing away metabolic waste in the brain.
By examining amyloid beta and tau protein levels (indicative of amyloid plaques and neurofibrillary tangles), this suggests that Alzheimer’s progression is due to the excess production and reduced clearance of amyloid beta and tau. Sleep then helps to facilitate this clearance, with lack of sleep disrupting it. However, whether sleep disturbance itself actually causes the development of Alzheimer’s is difficult to prove. Rather, combined with other factors (e.g. genetic, environmental, general health), poor sleep most likely exacerbates the progression of neurodegenerative diseases, or may serve as a catalyst that triggers neurodegenerative diseases in an individual who is already predisposed to it.
In any case, investigating the role of sleep in the development of neurodegenerative diseases is advantageous as addressing sleep-related issues can be relatively simple (e.g. sleep hygiene), non-invasive (e.g. CBT-I) and inexpensive—especially when combined with other therapies and treatments.
However, sleep not only affects your brain, but is associated with psychiatric and metabolic diseases, as well as certain cancers. By addressing and managing sleep issues before they become chronic therefore plays a key role in overall systemic health.
Tune in next Friday for another Sleep Science Friday and also check out a recent publication by ESRS member Zou et al. 2020 in the European Journal of Preventive Cardiology on Insomnia and metabolic syndrome.
Want to know more about sleep and neurological disorders? Further Reading:
- “Evaluating glymphatic pathway function utilizing clinically relevant intrathecal infusion of CSF tracer” (1 May 2013, Journal of Translational Medicine)
- “The Purpose of Sleep? To Forget, Scientists Say” (2 February 2017, The New York Times)
- “The glymphatic system in CNS health and disease: past, present and future” (8 February 2018, Annual Review of Pathology)
- “The Glymphatic System and Waste Clearance with Brain Aging: A review” (2019, Gerontology)
- “Vascular dysfunction—The disregarded partner of Alzheimer’s disease” (1 January 2019, Alzheimer’s & Dementia)
- “Increased glymphatic influx is correlated with high EEG delta power and low heart rate in mice under anesthesia” (27 February 2019, Science Advances)
- “Not all sleep is equal when it comes to cleaning the brain” (27 February 2019, Science Daily)
- “Brain Basics: Understanding Sleep” (13 August 2019, National Institute of Neurological Disorders and Stroke)
- “WHO factsheets: Dementia” (2020, World Health Organization)
- “Brain activity intensity drives need for sleep” (16 September 2019, Science Daily)
- “Interactive: Biomarkers in Blood Provide a Window into the Brain” (1 December 2019, The Scientist)
- “Sleep dysregulation, memory impairment, and CSF biomarkers during different levels of neurocognitive functioning in Alzheimer’s disease course” (4 January 2020, Alzheimer’s Researcher & Therapy)
- “To your health: sleep and the glymphatic system” (22 January 2020, KRCU)
- “Glymphatic System Impairment in Alzheimer’s Disease and Idiopathic Normal Pressure Hydrocephalus” (2020 March, Trends in Molecular Medicine)
- “Why do we need sleep?” (28 July 2020, The National Sleep Foundation)
- “One word protects your brain from diabetes and dementia” (29 July 2020, Psychology Today)
- “Inner Workings: A pulse of hope in the fight against Alzheimer’s” (4 August 2020, Proceedings of the National Academy of Sciences of the United State of America)
Interested in or working on sleep and sleep disorders?
Due to COVID-19, the 25th Congress of the ESRS goes Virtual–so you can attend even in your pajamas from anywhere worldwide.
For Spanish speakers, #ESRS2020 will be a joint congress with the Spanish Sleep Society. Both meetings are coordinated in parallel; attendants can participate in both meetings with only one registration. Keynote speakers from #ESRS2020 will have Spanish translations. We will also have poster sessions, teaching courses, networking lounges, and a stream for early career researchers.
All ESRS members are invited to participate in the ESRS Business Meeting and without registration for the ESRS Congress. Although, we encourage members to partake in the full Virtual Congress (Sept 22-24), with fees reduced at 50% of the normal cost. An invitation and agenda for the Business Meeting will be sent to members by 26 August.
During #ESRS2020’s Business Meeting, we will also be selecting new Board, Scientific Committee, and ESRS Early Career Researcher Network members! Please see here for further details on submitting nominations for open positions. We look forward to receiving your nominations.
Check out our full #ESRS2020 Scientific Programme on our website.
Just published an article? Want your research to be featured? Saw something interesting? Contact: doris.wu [ at ] esrs.eu.